For those of you who haven't heard about the Koestler Trust before, I;m glad that I get to be the first person to introduce such a brilliant charity to you.
The Koestler Trust is the UK's best-known prison arts charity. They have been awarding, exhibiting and selling artwork by offenders, secure patients and detainees for over fifty years now. Each year the trust put together a large art exhibition which is hosted by the Southbank Centre in London. Prior to the exhibition offenders, secure patients and detainees are invited to send in their art work - whether painting, sculptures or music and film etc. This year the trust received over 8000 entries, awards were given and the winning 120 pieces were displayed.
I am a massive lover of arts and crafts and am really interested in the way it can be used in Forensic settings. I am keen to use creative arts at work with my residents and have seen people really develop and grow through using the medium of arts and craft.
One of the best parts of using the creative arts as an OT is that it is easy to grade and adapt almost every creative medium to suit a whole range of individuals. Some brief examples of how I use creative arts where are work are as follows:
- Simple collaging techniques to improving fine motor skills.
- Utilizing creativity as a way of managing anger and aggression through residents channeling their emotions positively.
- Teaching new skills to increase confidence and self esteem.
- Creative arts as a way of assessment.
- Developing group skills.
- Using art to help residents discover their own personal identities, and talents.
There are so many benefits to utilising arts in OT and rehabilitation, and the aims of the Koestler trust in my opinion, definitely help support and encourage these benefits. The aims of the charity including helping offenders, secure patients and detainees lead more positive lives by motivating them to participate and achieve in the arts. Along side this the charity helps to increase public awareness and understanding of this group of society.
I had the privilege of taking a small group of residents up to see the exhibition this month and it was fabulous to see the art which was on display. Myself and the residents left the exhibition feeling inspired and full of ideas for our art groups and sessions back at work. What was truly priceless however was seeing how the art exhibition was helping to reduce the stigma and prejudices of offenders, detainees and in particular secure patients with mental health problems, through providing a safe yet emotive forum for the worlds offenders and the general public to mix.
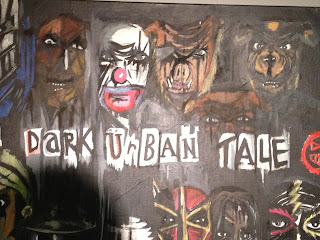
Here are a selection of photographs of the art work which the residents and myself liked in particular:
(Powerful words.)
(This sculpture is made purely from Soap - an every day object used to make something incredible!)
(This is a painting of an offenders dream house. What's interesting is that this is so similar to the dream houses which I have seen drawn and painted by different offenders since working in Forensics.)
(This intricate rose is made out of coloured pencil sharpenings. This individual has a talent from making the ordinary beautiful.)
I hope you have enjoyed looking at some of the photographs from this years exhibition. Sadly it is finished in London this year however there is always next year!
For more information on the Koestler Trust please take a look at their website below:
http://www.koestlertrust.org.uk/pages/uk2012/exhib2012.html
Happy OTuesday,
Kate :)